The gut microbiome plays a crucial role in the human body, affecting everything from digestion to immunity. One area garnering increasing attention is its impact on mental health, particularly in Major Depressive Disorder (MDD)—a leading cause of disability worldwide. Emerging research highlights the gut microbiome’s double-edged sword nature in both contributing to depression and offering new avenues for treatment.
Gut Microbiome and Depression: What Does Science Say?
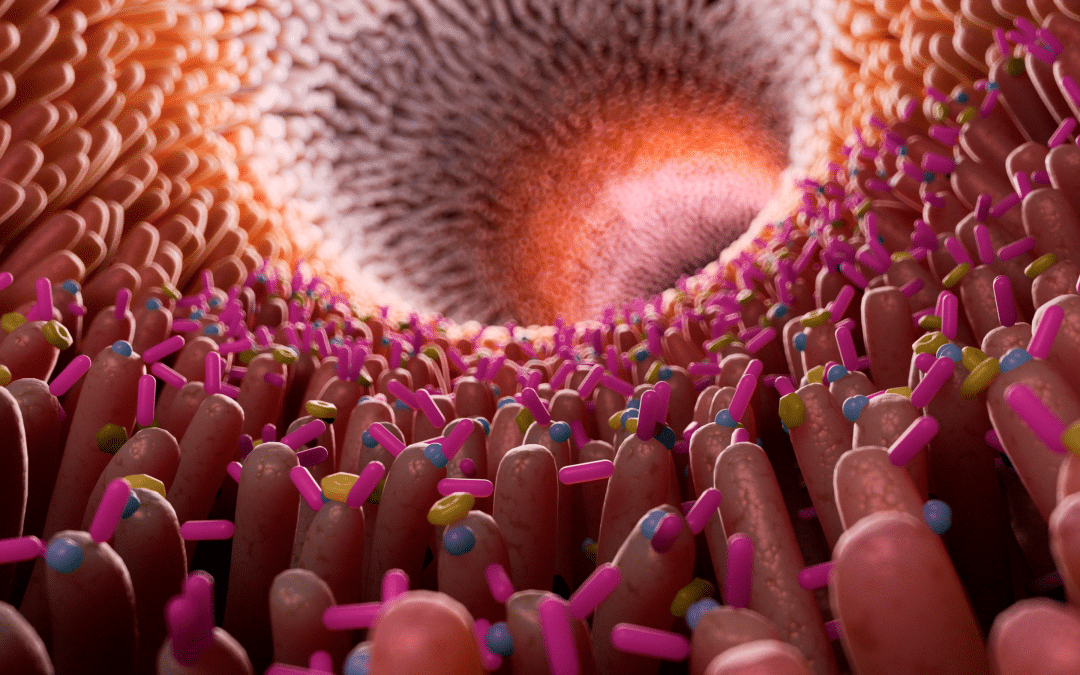
Systematic reviews indicate that changes in the gut microbiome’s composition and functions (e.g., metabolites) are closely linked with the onset and progression of depression through the regulation of the gut-brain axis. Dysbiosis, an imbalance in the microbial community, not only has a role in the pathogenesis of depression but also presents a novel therapeutic target. This suggests that while harmful bacteria and their byproducts may contribute to depression, they also offer a unique target for treatment.
Specific Bacterial Taxa and Their Influence on Mental Health
Studies have identified specific bacterial taxa that are commonly associated with mental disorders. For example, people with mental disorders often show lower levels of bacterial genera that produce short-chain fatty acids like butyrate, higher levels of lactic acid-producing bacteria, and increased bacteria related to glutamate and GABA metabolism.
Potential Strategies for Treatment
The gut microbiome is more malleable than genetic factors or social determinants, offering several potential treatment pathways:
- Modifying gut microbiota
- Altering microbiome metabolic output
- Targeting host responses to microbiome-derived factors
- Enhancing or blocking microbiome-mediated host mechanisms
Current research mainly focuses on the first two options, typically through probiotics or dietary strategies.
Latest Research Insights: Role of Proline and Probiotics
A recent study using mouse and fly models demonstrated that elevated blood levels of the amino acid proline, which are microbiome-dependent, correlate significantly with human depression severity. Too much dietary proline exacerbated depression in mice, whereas manipulating proline and GABA transporters genetically or using the probiotic bacteria L. plantarum offered protection against depression-like states in flies.
Gut Bacteria, Neurotransmitters, and Depression
Another groundbreaking study explored how gut bacteria might influence depression by producing neurotransmitters like serotonin and glutamate. The study also revealed a link between the gut microbiota’s composition and diversity and symptoms of depression. Notably, an abundance of the bacteria Eggerthella was identified as a potential cause of depressive symptoms.
Probiotics as an Emerging Treatment for MDD
While antidepressants remain the standard treatment for MDD, they don’t work for everyone and often have side effects like weight gain and sexual dysfunction. One of the first randomized controlled trials focusing on the microbiome-gut-brain axis suggests that short-term, high-dose probiotic supplementation can alleviate depressive symptoms, alter gut microbiota, and induce neural changes.
Final Thoughts: The Future of Probiotics in Depression Treatment
Advancements in research are slowly but surely demystifying the communication between bacteria and the brain. The targeted use of probiotics could soon become a precise science, potentially offering an effective alternative to traditional antidepressants. Profiling gut bacteria may even help identify individuals at risk for depression, paving the way for proactive treatment strategies.
By understanding the critical role of the gut microbiome in mental health, we can work towards more effective and accessible treatments for disorders like MDD.
Sources
[1] Liu, L et al. (2023) Gut microbiota and its metabolites in depression: from pathogenesis to treatment. eBioMedicine 90: 104527 https://doi.org/10.1016/j.ebiom.2023.104527
[2] Limbana, T., Khan, F., & Eskander, N. (2020). Gut Microbiome and Depression: How Microbes Affect the Way We Think. Cureus, 12(8), e9966. https://doi.org/10.7759/cureus.9966
[3] McGuinness, A.J., Davis, J.A., Dawson, S.L. et al. (2022) A systematic review of gut microbiota composition in observational studies of major depressive disorder, bipolar disorder and schizophrenia. Mol Psychiatry 27: 1920–1935. https://doi.org/10.1038/s41380-022-01456-3
[4] Shoubridge, A.P., et al. (2022) The gut microbiome and mental health: advances in research. Mol Psychiatry 27: 1908–1919; https://doi.org/10.1038/s41380-022-01479-w
[5] Mayneris-Perxachs et al., 2022, Cell Metabolism 34, 681–701 May 3, 2022 https://doi.org/10.1016/j.cmet.2022.04.001
[6] Radjabzadeh, D., Bosch, J.A., Uitterlinden, A.G. et al. Gut microbiome-wide association study of depressive symptoms. Nat Commun 13, 7128 (2022). https://doi.org/10.1038/s41467-022-34502-3